What is Pneumonia?What is the relationship between pneumonia and blood oxygen?
Respiratory illnesses, including pneumonia, remain a major concern to hospitals around the world, especially during the winter months when an influx of patients can put some hospitals into crisis mode.
Pneumonia ranges in severity from a mild illness to life-threatening. Anyone can contract pneumonia, but babies, young children and older people are particularly susceptible to the dangers of this illness (Healthdirect 2020).
Pneumonia is the leading infectious cause of death in children, with about 15% of deaths attributed to children under five (WHO 2019a).
What is Pneumonia?
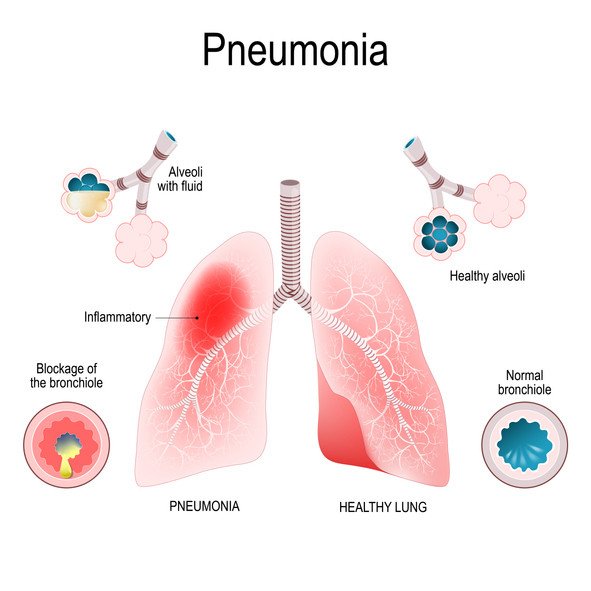
Pneumonia is an acute infection of the lungs that causes the alveoli in one or both lungs to fill with pus and fluids.

Pneumonia is an acute infection of the lungs that causes the alveoli in one or both lungs to fill with pus and fluids. This results in lung consolidation (wherein the alveolar spaces are filled with fluid instead of air) and interferes with gas exchange (Better Health Channel 2018; Moyer 2018).
When a person has pneumonia, breathing is painful and oxygen intake is limited (WHO 2019b).
Pneumonia doesn’t discriminate across the lifespan and can affect any age group, though it is more common in young children and older adults (Better Health Channel 2018). Depending on the severity, some people may not necessarily need to be hospitalised, whilst others will.
Generally, those with more comorbidities or any problem that may exacerbate pneumonia will require hospital admission. Pneumonia can also be treated in the community as long as the individual has access to good medical and nursing care.
How Serious is Pneumonia?
In the United States alone, approximately $10 billion is spent each year to manage about 4 million episodes of, and almost 1 million hospitalizations for, pneumonia.
In 2017, over two million people died from pneumonia worldwide (Dadonaite & Roser 2019).
Causes of Pneumonia
Pneumonia is caused by a viral, bacterial – or rarely – a fungal infection (Healthdirect 2020). In some cases, it is triggered by an existing cold or flu that enables pathogens to access the alveoli (Better Health Channel 2018).
Transmission commonly occurs by inhaling infected droplets in the air from a cough or sneeze of an infected person. It can also spread via blood (WHO 2019b).
Symptoms of Pneumonia
Symptoms may vary depending on age, the cause and severity of the infection, and any existing health problems (Better Health Channel 2018). Assessing the patient and gaining a comprehensive patient history is vital in diagnosis. Symptoms may include:
- Coughing (dry or productive);
- Fever, chills, or sweating;
- Breathing difficulties;
- Increased respiratory rate;
- Fatigue or general malaise;
- Little to no appetite;
- Chest pain;
- Abdominal pain or aches;
- Blue colouring around the mouth (cyanosis); and
- Nausea, diarrhoea, or vomiting.
(Health Direct 2018; Better Health Channel 2018; Healthy WA 2015)
With correct treatment, a health improvement is usually observed within 7 to 10 days (Better Health Channel 2018).
Symptoms of Pneumonia in Children
- Lethargy;
- Irritability;
- Chest pain;
- Abdominal aches or pain;
- Fever;
- Coughing and difficulty breathing;
- Little to no appetite; and
- Pallor.
(RCH 2018; Healthy WA 2015)
What is the relationship between pneumonia and blood oxygen?
Low oxygen saturation reflects an integrated noninvasive measure of the extent of lung parenchyma involvement by infection, consequent anatomic and physiologic derangements, and available cardiopulmonary functional reserve, and thus it seems to accurately capture the clinical severity of pneumonia.
Our results suggest that as a single independent criterion for hospital admission, oxygen saturation <92% might be both safer and clinically better-justified for patients with pneumonia.
-Clinical Infectious Diseases
Testing for fever, high pulse rate, crackly breath sounds, and low oxygen levels could be key to helping GPs distinguish pneumonia from less serious infections, according to a large study published in the European Respiratory Journal.
-ScienceDaily
How is Pneumonia Treated?
Antibiotics
Treatment depends on the severity of pneumonia. In mild cases, the individual may be able to take oral antibiotics in a community setting. For more severe cases, they may require admission to hospital and treatment with intravenous antibiotics, oxygen therapy and chest physiotherapy (Dunn 2005).
As pneumonia is an infection, antibiotic therapy should be started as soon as possible. Sometimes this can be before the causative organism has been determined, however, the type of antibiotic can be changed if necessary. Depending on the severity of pneumonia, this can be in either an intravenous or oral form (Watson 2008).
Oxygen Therapy
Another important aspect of pneumonia treatment is oxygen therapy and maintaining adequate oxygen saturation levels. Depending on the patient, oxygen saturation levels should be above 93%, with the oxygen concentrations also varying depending on the patient, their comorbidities and severity of pneumonia. Humidified oxygen therapy can also be used in order to assist the patient with expectoration (Watson 2008).
Sometimes pulse oximetry can be inaccurate on these patients, and this is where arterial blood gas levels may play a role in ensuring adequate oxygenation is being achieved. Some patients, even when receiving high flow oxygen, can still remain hypoxic, and therefore, continuous positive airway pressure may be indicated (Farrell & Dempsey 2013; Watson 2008).

Pain Management
It is important to remember that a patient with pneumonia may be in pain. This means that their lung expansion may be compromised, which can further exacerbate their condition. This pain can often be described as pleuritic-type chest pain (Farrell & Dempsey 2013; Watson 2008).
Those with severe pneumonia may require treatment from physiotherapists. As part of an interprofessional team, physiotherapists can assist in not only any concurrent physical decline and chest physiotherapy, but can also help teach the patient effective breathing patterns and posture to promote lung expansion and expectoration (Watson 2008).
Hydration
Other treatments for pneumonia should focus on ensuring the patient is adequately hydrated and if not, ensure that intravenous fluids are commenced. Adequate hydration is important for the expectoration of secretions and will also help with any associated hypotension. The individual may have increased fluid loss if they are febrile and continue to have an increased respiratory rate, therefore, urinary output should also be monitored, as this can flag deterioration in the patient’s condition (Dunn 2005; Watson 2008).
